| Title | PRELIMINARY RESULTS OF PROTECTIVE EFFECTS OF BIO-NORMALIZER AGAINST POST-OPEREATIVE COMPLICATIONS OF PHOTOREFRACTIVE |
|---|---|
| Year | 1999 |
| Author | Dr. Igor Ovechkin, Dr. Alexander Shakula, Professor Ludmila Korkina, |
| Publisher |
PRELIMINARY RESULTS OF PROTECTIVE EFFECTS OF BIO NORMALIZER AGAINST POST-OPERATIVE COMPLICATIONS OF PHOTOREFRACTIVE KERATECTOMY IN ACTIVE DUTY RUSSIAN MILITARY PERSONNEL
Clinical Investigators- Dr. Igor Ovechkin, MD, PhD, Dr. Sci., Head,
Ophtalmology Unit, 6th Central Military Clinical Hospital, Moscow, Russia
Signature
Dr. Alexander Shakula, MD, PhD, Dr.Sci., Head, Rehabilitation Department, 6th
Central Military Clinical Hospital, Moscow, Russia
Signature
Tel: (7095) 455 9300
Scientific Supervisor – Professor Ludmila Korkina, MD, PhD, Dr. Sci., Head,
Department of Molecular Biology, Russian State Medical University
Signature
Tel/Fax: (795) 434 7187
E-mail: korkin@a ha.ru
Moscow, 1999
Objectives
Standard optical devices (eyeglasses and lenses) are often inadequate to correct myopia in military personnel. Thus, myopic privates and on-duty-offices have difficulties in finding suitable refractive correction because of their wide variety of operational duties, including running, jumping, night driving, parachuting, swimming, etc. At the circumstances, spectacles quickly can become dirty and scratched in sandy, I marshy, or muddy terrain. Contact lenses offer some advantages, including compatibility with diving face masks, night vision devices, and parachute goggles. However, proper lens hygiene is very difficult or even impossible to maintain while in the field conditions. Furthermore, contact lenses may cause ocular discomfort during a typical period of continuous more than 24 hours activity. A safe and effective refractive surgical procedure could substantially benefit service personnel with myopia.
Simple non-complicated by astigmatism myopia has been successfully treated with photorefractive keratectomy (PRK) during last decade. The details of PRK surgical procedure and reports of numerous clinical trials have been published worldwide (1-4).
Despite the ability to reduce myopia and improve uncorrected vision, there are unanswered questions regarding the “quality of vision” and some complications such as slow healing process, pain and haze in the post-operative period.
This study aimed to prevent or ameliorate some common complications after PRK surgery using a short-term systemic and topical Bio-Normalizer application.
Clinical study design and patients’ assessment
Forty male service men underwent PRK for the correction of myopia. The protocol and case report form of the clinical study (PRK operation and post-operative procedures) were approved by the Etique Committee of the 6’h Central Military Clinical Hospital, Moscow, Russia. Eligibility criteria included a stable refractive error between -1.5 and -6 diopters, D (Group I, 23 patients) and -6 to – 11 diopters (Group II, severe near sighting, 17 patients). All participants were with no more than 1 D of astigmatism, normal ocular health, and intolerance to eyeglasses and contact lenses. Subjects had to be 21 years of age (mean age 26±6 years, age range 21 -44 years) or older and active-duty military. Hard contact lenses users were required not to wear the lenses for at least 3 weeks before the preoperative period. For those with soft lenses the refraining period was 1 week before the PRK operation.
Informed consent was obtained from each participant after an extensive question and answer session on PRK itself and Bio-Normalizer in particular, including risks, benefits, and alternatives. The research purpose of the study was explained in details. All participants were given 1 sachet of BN one hour before the operation and 1 sachet of BN one hour after the PRK. Then, the patients received topical BN application (as 5% and 10% drops, 2 drops x 5 times a day for 4 days after operation) to experimental eye. The control eye of the same patients received the solution of “artificial” tear (2 drops x 5 times a day for 4 days after operation).
All photoablations were carried out by an experienced refractive surgeon (Igor Ovechkin, MD, PhD, Dr. Sci.) With the 193 nm ES-5000 excimer laser (NIDEK, Japan) using a 6-mm diameter ablation zone. According to manufacturer information the lazer delivered an intermittent energy density of 180 mJ/cm2 a pulse repetition rate of 10Hz, and an ablation depth of 0.25 μm/pulse. Total ablation depth was determined by the NIDEK algorithm after the refractive data were download to the lazer. The patients’ pupil was constricted, and anesthesia was obtained with topical procaine. Then, several lazer pulses were applied onto the corneal epithelium. The destroyed epithelium was removed with a blunt spatula to clear the central 6-mm zone. Finally, corneal surface was smoothed with metylcellulose and dried with a sponge. Postoperatively, the patients received conventional therapy with ointment and drops. Additionally, the experimental eye received BN drops according to above scheme.
Postoperative testing.
The patients were examined daily until complete re-epithelization. To evaluate the efficacy of BN, the examinations consisted of: (1) uncorrected visual acuity; (2) postoperative pain; (3) duration of full re-epithelization; (4) postoperative haze.
Results.
The mean values of baseline myopia for experimental and control eyes and operative intervention to both eyes did not differ each from other (Table 1).
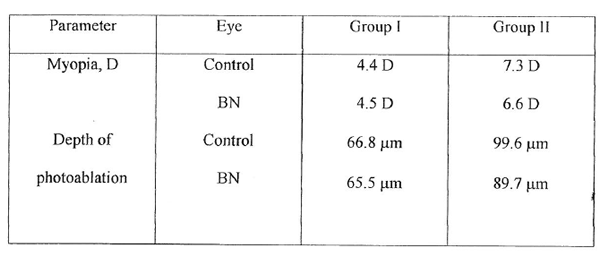
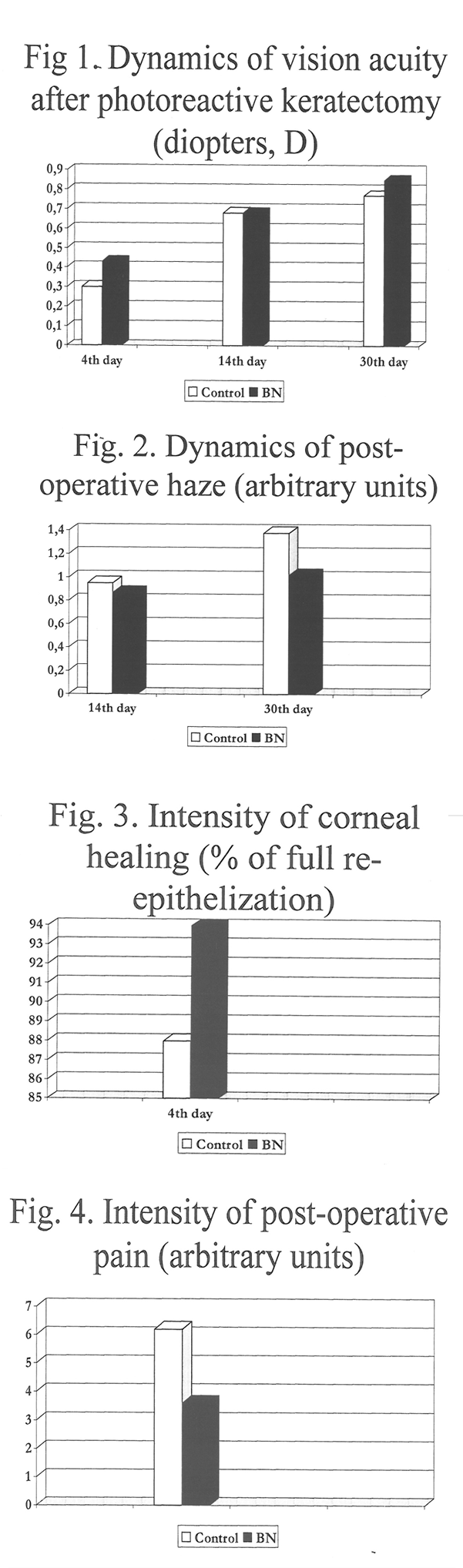
The preliminary phase II clinical investigation revealed positive therapeutical effect of combinatory (systemic and topical) BN administration to military men subjected to PRK (Fig. 1-8). The vision acuity in the experimental eye of the first group of patients was 0.13, 0.02, and 0.08 D higher than in the control one at the 4th, 14th and 30th day, respectively. The score of post-operative haze was 0.08-0.36 arbitrary units lower than in the control eye. The pain in the operated eye was 1.7-fold less intensive in the experimental vs control eye. The BN-induce improvement of corneal healing was proven by the increased number of complete re-epithelization by the 4th day after operation (Fig. 1 -4). In the second group of patients with severe myopia, BN administration increased vision acuity (or decreased a degree of non-corrected myopia) by 0.08, 0. 1 , and 0.07 0 at the 4th, 14th and 30th postoperative days, The haze decreased (by 0.12-02 arbitrary units ) and the ocular pain was less intensive for the experimental eye (11 % difference between the groups). The corneal healing was completed by the 4th day after operation in 91% of patients of the experimental group and in 84% of the control patients (Fig. 5-8).
Conclusions.
The preliminary results of the trial allowed us to suggest that BN prescribed both in powder and eye drop forms to the patients subjected to PRK could improve the quality of vision and diminish the frequency and intensity of post-operative complications. However, the optimization of the scheme of BN pre- and post operational administration has to be further evaluated.
References.
- Schallhorn S.C., Blanton Ch. L., Kaupp S.E., Sutphin J., Gordon M., Goforth H., and Butler F.K., Ophthalmology, 1996, 103, 5-22
- Lanzetta P., Menchini U., and Virgili G., Br. J. Ophtalmol, 1999, 83,29-32
- Thomas J.V., Simmons R.J., and Belcher C.D., Ophthalmology, 1982, 89, I 87-197
- cDonald M.B., Liu J.C., Byrd, T.J., et al., Ophthalmology, 1991, 98, 1 327-1337
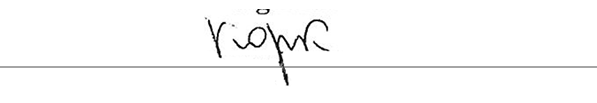
Table 1 Baseline characteristics for clinical groups